Glossary
CRS Child Restraint Systems
NDIS National Disability Insurance Scheme
Introduction
Road vehicle crashes are one of the leading causes of death in children (Australian Institute of Health and Welfare, 2019; Cunningham et al., 2018). The implementation and appropriate use of child restraint systems (CRS) are proven to reduce the incidence of injury and fatality among children (Arbogast et al., 2009; Sauber-Schatz et al., 2014). Safely transporting children in vehicles requires that they be comfortably and securely restrained in a CRS suited to their size and individual needs because inappropriate use of CRS increases the risk of a child becoming injured (Brown et al., 2006; Lesire et al., 2007).
Children with disabilities and medical conditions are at an increased risk of being inappropriately and inadequately restrained in CRS, placing them at additional risk of injury or fatality when travelling (Downie et al., 2019). Here, we use disability and medical conditions to broadly capture the range of conditions that may impact a child. Disability refers to diagnosed developmental, cognitive, or physical conditions that interfere with an individual’s functioning in their everyday life (e.g., autism or cerebral palsy) due to a poor match between an individual and their environment, while medical condition refers to physical injuries, illness, or conditions (e.g., heart conditions). Off-the-shelf CRS may not be suitable for children with disabilities and medical conditions who may have different physical or behavioural needs than their peers (Downie et al., 2019). Conditions impacting posture and movement, orthopaedic conditions, and medical conditions that may necessitate medical equipment, can influence a child’s ability to sit and be adequately supported in typical off-the-shelf CRS (Downie et al., 2019). The use of wheelchairs as in-vehicle seats can introduce additional complexities associated with ensuring the wheelchairs are appropriate for transport and adequately secured (Buning & Karg, 2011; Fuhrman et al., 2010; Yonkman et al., 2010). At the same time, children may show complex behaviours resulting from differing emotional, communication, or sensory needs, which may increase the risk of children escaping a CRS or injuring themselves and others in the vehicle (Plummer et al., 2021; Yonkman et al., 2013).
Ensuring the safe transportation of children with disabilities and medical conditions is indeed a complex issue. It involves families, professionals, and organisations (including government agencies), and is influenced by a multitude of factors, including attitudes, policies, technology, and design (Ross et al., 2020). While caregivers are involved in the day-to-day transportation of their children, health professionals and organisations are often involved in supporting the caregiver to choose and source suitable equipment for their child, accessing funding for equipment, installing equipment, and educating caregivers on how to use it appropriately and safely (Baker et al., 2012).
Australian standards, such as the Restraint of Children with Disabilities, or Medical Conditions, in Motor Vehicles (AS/NZS 4370:2013), provide health professionals and organisations with guidance on the prescription of CRS for children with disabilities. However, health professionals and people involved in the safe transportation of children with disabilities and medical conditions must often identify suitable CRS to accommodate the needs of these children. This includes specialist CRS that may not comply with the Australian standard for child restraints (AS/NZS 1754). Research conducted in Australia in 2012 identified that occupational therapists had a limited understanding of AS/NZS 4370 and faced challenges in making recommendations to support the safe transportation of children with disabilities (Baker et al., 2012).
While it is known that transporting children with disabilities and medical conditions is associated with additional risks, limited research exploring the knowledge and challenges of allied health professionals exists (Baker et al., 2012). Little is known about how health professionals and organisations are currently working to support the transportation of these children, their perceived knowledge and confidence in supporting families, and where and how they are obtaining information to underpin clinical decisions. A large-scale survey was recently conducted to explore the transportation of children with disabilities and medical conditions from the experiences and perspectives of their caregivers (Black et al., 2023). The present study focuses on the experiences and perspectives of the health professionals and relevant organisations who carry out work in this area, such as those who supply or fit specialised CRS or who may assist with, or be responsible for, some element of transporting these children, such as school bus services, disability support agencies, and transport related government departments.
Method
Design
This study was part of a larger project conducted in collaboration with Mobility and Accessibility for Children in Australia Ltd (MACA; https://www.macahub.org) examining safe transport for children with disabilities and medical conditions. Previously reported were the experiences of families and caregivers (Black et al., 2023). Here we conducted a national Australian survey to explore the experiences, perspectives, and knowledge of health professionals working with children with disabilities and medical conditions and organisations with responsibilities relating to transporting these children. An online survey was deemed appropriate to enable a broad range of experiences across Australia to be collected (Ball, 2019).
Materials
As no survey exists on this topic, a survey was designed by the research team for the purposes of this study. The survey was designed by researchers and clinicians working in the field/area in collaboration with experts in road safety for children with disabilities. The survey was piloted with caregivers of children with disabilities before its use. A complementary survey designed for families and caregivers has been reported elsewhere (Black et al., 2023). The large-scale survey used two different questionnaires, one for health professionals and one for organisations. The health professional survey included questions on demographics including practice area and background, and questions regarding assessment, recommendation (advise or suggestion) and prescription (to prescribe or specify equipment) practices, knowledge and beliefs, challenges in addressing seating needs and accessing information. The organisation survey included questions on demographics, such as organisation type and size, and explored organisational knowledge and beliefs including questions on the organisation’s plan and strategies, involvement in research activities and access to information. Both the health professional and organisation surveys consisted of single and multiple-choice response options, Likert scales (all scales reported on 0-10 scale) and open-ended questions. The survey for health professionals comprised 28 items while the survey for organisations comprised 14 questions.
Procedure
The survey was distributed online via the online survey platform, Qualtrics (2005), with respondents provided with the option to register to complete the survey via telephone or mail. Participants were given information about the study and were required to provide informed consent via the online survey platform. Participants automatically entered the draw to win one of three $50 vouchers as a token of appreciation for their time. Data collection was completed between July 2020 and May 2021. The median completion time for the health professional survey was 12 minutes (interquartile ranges (IQR): 9.5), while the median completion time for the organisation survey was 7.4 minutes (IQR: 9.1).
Recruitment
Individuals were eligible to participate if they were based in Australia and were 1) health professionals with experience working with car seating and other transportation needs of clients with disabilities and/or medical conditions under the age of 16 years, or 2) organisations or government representatives with an interest in, or responsibility for the transportation of children with disabilities and medical conditions. Participants were recruited through social media, therapy and disability organisations and providers, contact lists of participants who had previously registered to participate in research, and networks of the research team.
Data analysis
Data were exported from Qualtrics and imported into SPSS Statistical software (IBM Corporation, 2020) for data cleaning and analysis, using descriptive statistics and frequencies, with medians (MDN) and IQR presented for Likert-scale data, which provided a measure of central tendency and variability. Health professionals’ and organisations’ postcodes were used to provide a measure of practice area socio-economic status. The Index of Relative Socio-economic Advantage and Disadvantage (IRSAD) based on the Australian Government Socio-Economic Indexes for Areas (ABS, 2016) was used, whereby areas are ranked on scale of 1 to 10. Higher scores equate to greater advantage and lower to disadvantage. Results are reported separately for health professionals and organisations. In the health professional survey, respondents could select “other” and provide free-text responses. These responses were examined and, in some cases, text provided by health professionals were used for demonstrative purposes.
Results
Participants
A total of 305 individuals, including 243 health professionals and 62 organisations accessed the survey. Respondents were required to complete at least 50 percent of the survey to be included in the analysis, with 10 responses being excluded from the analysis due to insufficient completion. A total of 295 responses were included in the analysis, comprising 234 health professionals and 61 organisations.
Demographic characteristics of the sample are displayed in Table 1. Health professional respondents were primarily Occupational Therapists, followed by Physiotherapists, and other health professionals. Health professionals worked with a variety of children with disabilities and medical conditions. As shown in Table 2, the most common condition was Cerebral Palsy, followed by Autism Spectrum Disorder and Global Developmental Delay or Intellectual Disability. Respondents representing organisations were from a variety of sectors, most frequently representing disability organisations, health service providers, transport agencies and regulators (Table 1).
Health professionals
Assessment, recommendations and prescription practices
Health professionals most frequently reported addressing the seating or transport needs of children with disabilities and medical conditions occasionally (39.8%) or monthly (30.6%), followed by weekly (17.3%). A proportion of health professionals reported addressing transport needs daily (4%), while 8.4 percent reported rarely addressing such transport needs. Most health professionals reported always assessing seating needs in an initial assessment (25.3%), almost always (29.5%), usually (17.8%) or sometimes (18.2%), while 8.4 percent and 0.9 percent reporting doing it almost never, and never, respectively. Harnesses were the most commonly prescribed or recommended device (68.2%), followed by special purpose CRS (63.2%), commercially available off-the-shelf child restraints (60.1%) and buckle-guards (57%). Chest cross straps (40.8%), additional padding (39.5%) and head support (36.8%) were also commonly recommended or prescribed by health professionals. Some (13.9%) reported prescribing or recommending other systems.
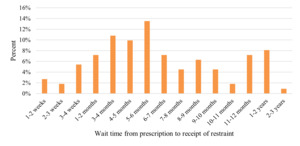
Health professionals who had prescribed a special purpose CRS funded by the disability Insurance Scheme (NDIS) were asked to report on the wait times for a recent instance where they had prescribed a special purpose CRS (n=111). The wait time from point of identification to receipt of the CRS varied between 1-2 weeks to 2-3 years with the most frequently reported wait time being 5 to 6 months (Figure 1). In 3.4 percent of cases (n=8) health professionals reported prescribing a special purpose CRS but funding was not approved. When prescribing special purpose CRS, health professionals (n=183) reported that in most cases the supplier fitted the special purpose CRS (45.5%), with caregivers and car seat fitters fitting the special purpose CRS 13.7 percent and 10.9 percent of the time, respectively. The health professional reported fitting the special purpose CRS themselves 7.1 percent of the time, while 10.9 percent of health professionals did not know who fitted the special purpose CRS. Other methods of fitting special purpose CRS were also reported by health professionals (9.4%), which was most frequently the health professional and supplier or fitter fitting the special purpose CRS together.
Once a special purpose CRS had been prescribed, health professionals varied in the frequencies that they reviewed a child’s transportation needs, but most often within 6-12 months (28.6%). Some health professionals conducted reviews earlier than 6 months (27.8%), reviewing seating needs in less than a month (5.1%), within 1-3 months (9.8%) or between 3-6 months (12.8%), whereas others reported reviewing seating needs beyond a twelve-month period (12%). One in eight (12.8%) never reviewed seating needs once a special purpose CRS was prescribed. For health professionals whose clients transition into adult services (n=74), most health professionals included a handover of the child’s seating or transportation needs (68%), while 32 percent did not.
Health professional knowledge and beliefs
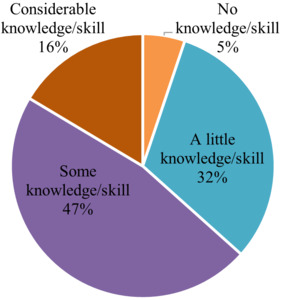
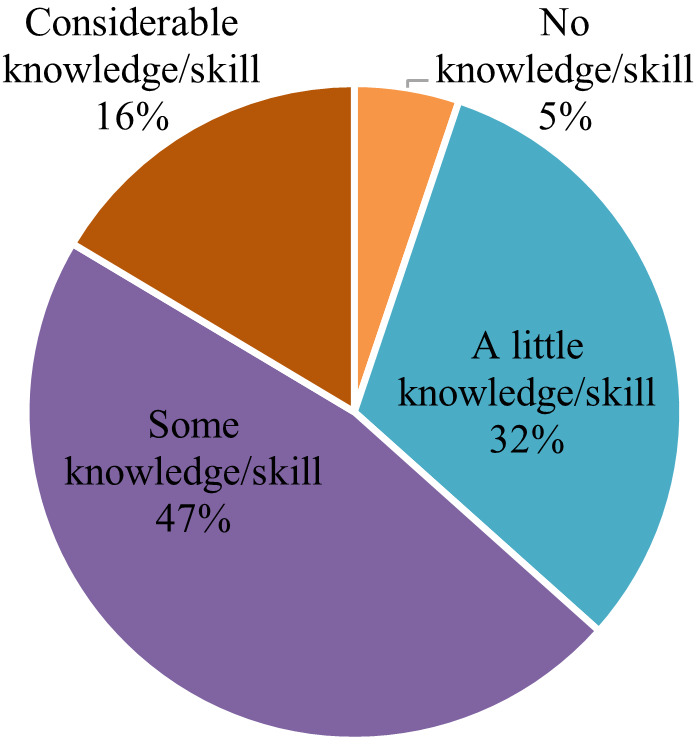
When asked to rate their level of agreement that children with disabilities and medical conditions had the same rights as other children to safe transportation on a 0-10 point Likert scale (greater scores indicating higher levels of agreement), the majority of health professionals strongly agreed (MDN=10, IQR=0). While 16.4 percent of health professionals believed that they had considerable knowledge and skill in addressing the car seating needs of children with disabilities and medical conditions, health professionals most frequently believed that they had some (47%) or a little knowledge or skill (31.5%), as shown in Figure 2.
When asked to rate their confidence in their level of knowledge on a 0-10 point Likert scale (with a greater score indicating more confidence), health professionals’ confidence varied. They were most confident in their knowledge of the road laws for travelling in a motor vehicle for children without disabilities (MDN=7, IQR=4), and with disabilities (MDN=6, IQR=5) in their own state or territory. In other states and territories, health professionals had lower confidence ratings for both children without (MDN=3, IQR=5) and with (MDN=2, IQR=5) disabilities.
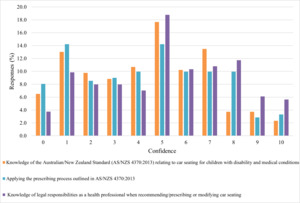
As shown in Figure 3, health professionals were somewhat confident in their knowledge of their legal responsibilities as a health professional when recommending/prescribing or modifying car seating (MDN=5, IQR=4), their knowledge of the Australian/New Zealand Standard (AS/NZS 4370:2013) relating to car seating for children with disabilities and medical conditions (MDN=5, IQR=4), and the prescribing process outlined in the standard (MDN=5, IQR=5) when asked to rate their confidence (higher scores equate to greater confidence).
Fewer than half of health professionals reported having access to the Australian/New Zealand Standard 4370:2013 Restraint of children with disabilities, or medical conditions, in motor vehicles (45.3%), 3.8 percent reporting that they did not know what this standard was, and 5.6 percent of the sample did not respond to this item.
Challenges in addressing seating needs
The majority of health professionals reported that they had experienced challenges when recommending or prescribing car seating for children with disabilities and medical conditions (92.4%). Over half reported that a lack of appropriate training and professional supports, a lack of specialised knowledge, and a lack of appropriate seating options were challenges, as shown in Table 3.
Other challenges were also commonly reported, including a lack of trial options for families, and managing issues around car seats, restrictive practices, and manual handling. They also noted a lack of comprehensive and clear guidelines and resources, and a lack of a central point for information were challenges.
"Lack of comprehensive and clear guidelines for decision making that is accessible to all stakeholders (especially funding bodies) since response to specialised car restraints/ accessories varies depending on who you speak to and their personal understanding. This increases the time taken for the application process due to back and forth, even if clear justification has been provided. Funding bodies are understandably apprehensive about approving items for transport that don’t strictly meet the standard/crash tested and many disability related items don’t fit this criteria [sic]. "
"No central point to go to for information – often trawling through different databases, government departments, websites etc. to try to get all info together and trials, required documents completed. "
Accessing information
When asked in a multiple choice question where multiple options could be selected, health professionals most frequently reported obtaining their knowledge and skills about addressing car seat and travel needs for clients (under 16 years) with disability/medical conditions from other health professionals (81.7%), followed by reading standards and guidelines (66.7%). Over half reported learning from the supplier of special purpose seating options (57.7%), while 39.4 percent reported learning through trial and error. Health professionals also reported learning through online (21.1%), short course or professional development options (20.2%) and other options (20.2%), such as professional networks, organisations and websites. Tertiary education was the least frequently reported source of knowledge and skills (7.5%).
The majority of health professionals reported that they had previously accessed information, support or advice regarding transport for children with disabilities and medical conditions (76.5%). Health professionals most commonly accessed information via a laptop computer (49.6%), or a desktop computer (32.1%), whereas a small proportion used a mobile phone (4.7%) or a tablet (3%).
When asked where they would like to receive information on the safe transport of children with disabilities and medical conditions, they endorsed a range of modalities (multiple options could be selected). Online training (84.7%), websites (78.9%), and short courses or professional development events (77.5%) were most frequently endorsed. Nearly half of health professionals reported a desire to obtain information from a senior health professional (49.3%), or a telephone advisory service (45.5%). Brochures (33.5%), mainstream shops (18.2), and other sources (8.1%) were also endorsed.
Health professionals, when asked in a multiple choice question where multiple options could be selected, believed that the easiest source of information for caregivers to access on the safe transportation of children with disabilities was from allied health professionals (85.5%) or websites (72%). Health professionals also endorsed disability service providers (41.1%), mainstream shops (33.8%), social media (26.1%), telephone advisory services (24.0%), early childhood services (18.8%), schools (18.4%), hospitals (19.3%), doctors (20.8%), and maternal and child health services (15.5%) as sources of information for caregivers. Some also endorsed other sources of information (6.3%) such as dedicated organisations.
Organisations
Organisation knowledge and beliefs
When asked to rate their level of agreement that children with disabilities and medical conditions had the same rights as other children to safe transport on a 0-10 point Likert scale, the majority of respondents from organisations strongly agreed, (MDN=10, IQR=0).
Most organisation representatives were aware of the Convention on the Rights of the Child (80.3%) and the Convention of the Rights of Persons with Disabilities (85.2%). Organisational representatives were also aware that there are CRS made specifically for children with disabilities and medical conditions (85.2%). Over half (67.2%) of organisations were aware of the Australian/New Zealand Standard (AS/NZ 4370:2013). The vast majority of representatives from organisations were aware of the road laws relating to motor vehicle transportation for children with disabilities in their state or territory (88.5%), however, fewer were aware of road laws in other states or territories (50.8%).
Organisations’ strategies or plans included safe transportation for children with disabilities and medical conditions in 34.4 percent of cases, while 8.2 percent did not. Some representatives were unsure whether addressing this was included in their organisation’s strategy or plan (18%), while 31.1 percent of organisations did not have a strategy or plan. Five respondents (8.2%) did not respond to this item.
Organisations believed that a range of agencies were accountable for ensuring the transportation needs of children with disabilities and medical conditions were met when travelling. The most frequently endorsed organisation believed to be accountable for ensuring the safe transportation of children with disabilities and medical conditions was the NDIS (63.9%), followed by transport agencies or regulators (62.3%), State or Territory governments (55.7%), Commonwealth government (55.7%), disability organisations (44.3%) and local governments (27.9%). Some organisations suggested other approaches (18%) including families, law enforcement, schools and transport equipment providers.
Over the previous 12 months, 37.7 percent of organisations had undertaken research or activities to support the safe transportation of children with disabilities or medical conditions, 41 percent had not, while 13 percent of representatives were unsure. Five respondents (8.2%) did not respond to this item.
Accessing information
Organisations believed that information about how to safely transport children with disabilities or medical conditions should be available from a range of sources. The most frequently endorsed avenues were websites, government or non-government websites and allied health professionals, as shown in Table 4.
Discussion
The findings from these two surveys indicate that health professionals and organisations involved in the transportation of children with disabilities and medical conditions strongly believe safe transportation is an essential right for all children. However, health professionals’ confidence in their knowledge in this area is often insufficient to adequately support these children and their families. This is perhaps of note given that nearly half of health professionals (43.6%) reported having over ten years’ experience in the field. Furthermore, only a third of the organisations reported having a strategy or plan that specifically addressed this topic. This study highlights the persistent challenges and knowledge gaps of health professionals and organisations, leading to children with disabilities and medical conditions being exposed to disproportionately high risks of injury and fatality in road vehicle transportation (Downie et al., 2019; Falkmer et al., 2001). Given that children are at an increased risk of injury and fatality during road vehicle transport (Cunningham et al., 2018), improving the transport safety of children has been a global priority (WHO, 2020).
While caregivers are predominantly responsible for the everyday transport of their children with disabilities or medical conditions (Black et al., 2023), health professionals and organisations play an important role in providing information and specialised support. The health professionals’ varying confidence in their knowledge regarding the seating needs of these children during transport is therefore a concern. A considerable proportion of caregivers cited a lack of appropriate training and support as a challenge to addressing these needs. Despite the vast majority of survey participants holding a tertiary (university) degree in the fields of health or medical sciences, tertiary education was the least frequently reported source of knowledge and skills in this area, which could easily be mitigated with the topic being made a mandatory part of the curricula. Previous research focusing on the safety of children with Autism Spectrum Disorder during transport concluded that tertiary education programs for relevant health professions, such as occupational therapy, should place greater emphasis on transport needs of individuals with disabilities in their curricula (Yonkman et al., 2013). Given the present study, the absence of tertiary education in teaching health professionals these essential skills is concerning, especially as research a decade ago identified a lack of knowledge as a key challenge faced by health professionals involved in supporting the transportation of children with disabilities and medical conditions (Baker et al., 2012). Including additional education in tertiary education may not be the only solution; for example, professional development or online sources may also support health professionals to develop skills. Further, websites that provide advice or information were also strongly endorsed by health professionals as a means to obtain information to support them in addressing the transport of children with disabilities and medical conditions. Regardless of source of information, health professionals require additional resources, to develop their skills and confidence to support caregivers with their child’s needs during transportation. Based on the data in the present study, it is clear that health professionals are seeking to understand more about the transport options for these children, indicating a need to engage in further study, such as online or professional development courses.
Critically, fewer than half of health professionals reported having access to the Australian/New Zealand Standard 4370:2013 Restraint of children with disabilities, or medical conditions, in motor vehicles, with a minority not being aware of this Standard. This is of concern given that health professionals have important legal and ethical obligations to ensure that their clients are transported appropriately. This finding replicates those of a study conducted ten years ago, indicating that little has changed to support health professionals to ensure that they have the knowledge and confidence to fulfill their legal responsibilities and to support families to ensure that their children are being transported appropriately (Baker et al., 2012).
The present study also indicates that alongside challenges associated with understanding best-practice and legal requirements, factors including access to appropriate CRS and trial options were challenges faced by health professionals when prescribing such systems. In Australia, there is limited access to a suitable range of special purpose CRS and no evidence-based information about their safety performance and best practice use, restricting the ability of health professionals to recommend a special purpose CRS that may be more appropriate for the child. Furthermore, the cost of special purpose CRS is often prohibitive for families (Bourke-Taylor et al., 2015). However, Australia’s established NDIS provides funding for special purpose CRS for eligible participants. Without access to evidence-based information, suitable products, and adequate trial options, the ability of health professionals to appropriately support children’s safe transport needs is negatively impacted, placing children and their families at additional risk of injury or fatality.
The organisations believed the NDIS to be primarily responsible for the safe transportation of children with disabilities and medical conditions. However, multiple other bodies were also identified as accountable for meeting the unique needs of this population during travel. Despite their perceived role in ensuring the safe transportation of these children, many organisations neither had strategies or plans in place, nor had undertaken any research or activities supporting the safe transportation of children with disabilities and medical conditions in the previous 12 months. These data suggest an uncertainty among organisations about their role, and also how specific organisations can further support safe transportation of these children.
Among organisations, websites were the most commonly cited source of safety information regarding transport of children with disabilities and medical conditions. Although caregivers reportedly preferred obtaining information from a website, second to health professionals, the percentage of caregivers who actually received information from a website was indeed very low (5.2%) (Black et al., 2023). This finding suggests there may be some disparity between awareness and availability of information, and that organisations can play a more significant role in directing caregivers to relevant information, including online sources.
Strengths and limitations
This study provides a national update on the continuing gaps in information and training for health professionals engaged in transporting children with disabilities and medical conditions. This work builds on existing research that clearly establishes that more resources are needed to fill this gap for these supporters of this group of vulnerable road users. The study also provides the clarity about how health professionals are interested, and currently seeking, information. The findings provide many of the answers as to what information is needed with the clear list of challenges for health professionals. The insights also give information providers (e.g., NDIS, CRS manufacturers, support organisations) direction regarding how and where to provide information that will be accessible to health professionals.
The findings of the present study should be interpreted with the following limitations. Firstly, this study was conducted in Australia and while applicable to other countries with similar contexts, it also limits the generalisability of findings to other countries and systems and contexts. As participation in this study was voluntary, results may be biased to those health professionals and organisations who hold strong views on the topic (Elliott & Valliant, 2017), and may not generalise to other professionals and organisations. Despite these limitations, this study provides a comprehensive overview of challenges, beliefs and availability of information relating to transport of children with disabilities and medical conditions.
Conclusions
The present study highlights gaps in the knowledge of health professionals and organisations involved in supporting the transportation of children with disabilities and medical conditions. Although key stakeholders believe the safe transportation of these children to be an important right, health professionals have low confidence in their abilities to address the barriers associated with their transportation. There is potential for health professionals and organisations to be better supported in this area, in order to fulfill their significant role in providing caregivers with both information and practical assistance relating to the transport of children with disabilities and medical conditions. The findings also suggest that health professionals may benefit from additional training, professional development, and easy access to resources to better meet the needs of their clients. Organisations need access to evidence-based information to address this transportation topic in their strategies and plans. Without addressing the barriers identified in this research, and improving support for health professionals and organisations to increase their knowledge in this area, children with disability and medical conditions and their families will remain at a disproportionate risk of injury and fatality on the roads.
Acknowledgements
We would like to extend our gratitude to the health professionals and organisations who participated in this study.
Author contributions
Project conception: MHB, TF, HE, EC. Funding acquisition: TF, HE, EC. Supervision: MHB. Investigation: MHB, MHE, TP. Data curation: MHB, MHE, TP. Formal analysis: MHB. Interpretation of Results: All authors. Writing - original draft: MHB. Writing - critical revision for intellectual content: All authors. All authors have read and agreed to the published version of the manuscript.
Funding
The present study was funded by the Australian Government, Department of Social Services and supported by the Australian National Disability Insurance Agency. It is part of a larger project seeking to develop and evaluate a national Australian resource to support the safe transportation of children with disabilities and medical conditions.
Human Research Ethics Review
The study protocol was approved by the Curtin University Human Research Ethics Committee (HRE2020-0257).
Data availability statement
Data is available upon reasonable request.
Conflicts of interest
The authors declare that there are no conflicts of interest.